Trusted Medical Credentialing Services
We provide medical credentialing services to simplify healthcare provider
enrollment. Get credentialed and enrolled twice as fast, twice as easy!
We provide medical credentialing services to simplify healthcare provider
enrollment. Get credentialed and enrolled twice as fast, twice as easy!
Medical credentialing is a complex process where even minor errors or missing details can delay provider enrollment. However, our validated and certified process ensures hassle-free enrollment with insurance networks. We provide an intuitive platform designed to save time, ensure compliance, and keep credentials up-to-date for all kinds of healthcare practitioners. So, if you want seamless credentialing, gather your documents and get started today.
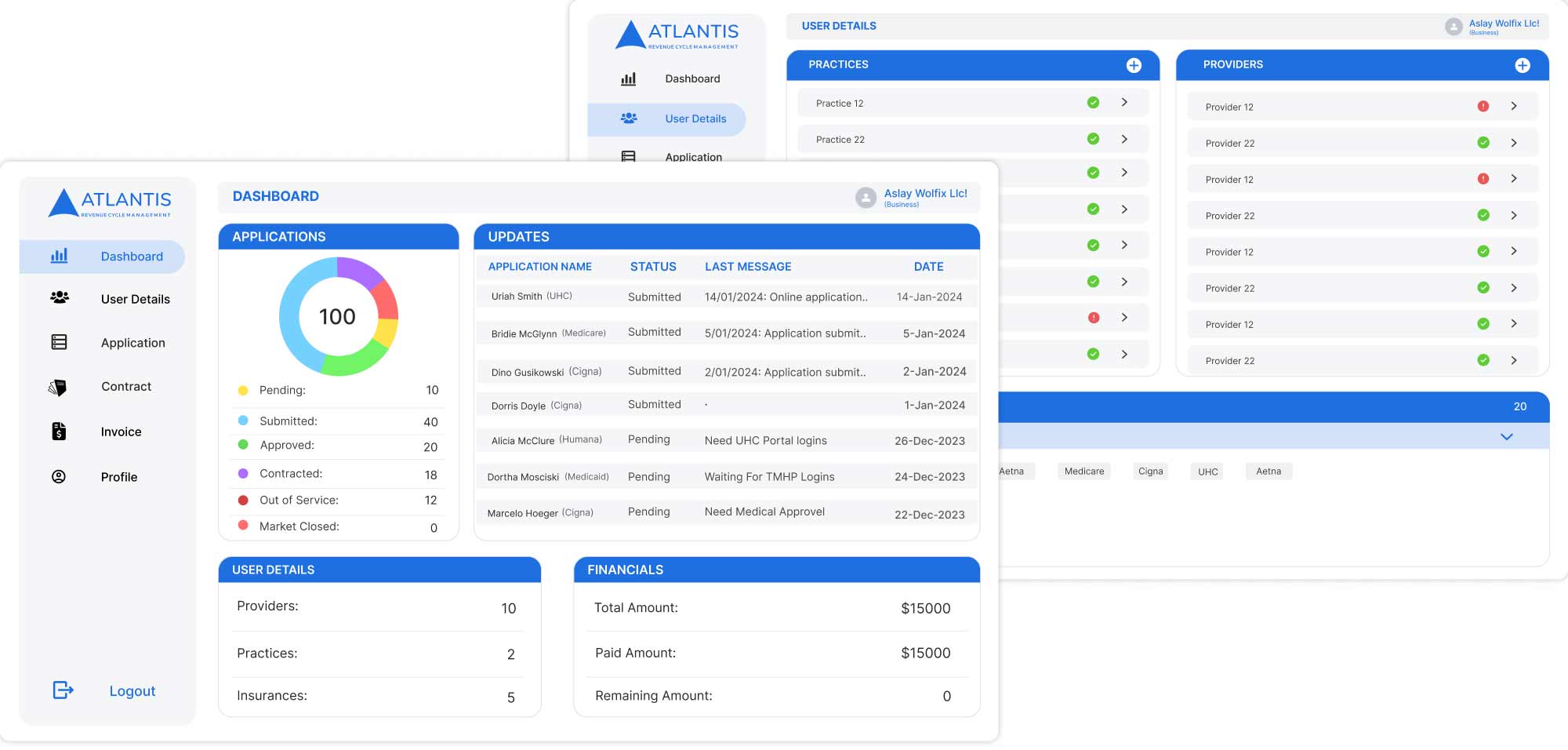
Get credentialed first—because without credentials, there are no payments! We handle the provider credentialing process, from verification to premium network enrollment. This allows you to enroll with major insurance providers, including CMS/Medicare, Humana, Cigna, and Aetna. With an efficient and personalized process, we save your time, boost your practice revenue, and eliminate administrative headaches. Our comprehensive support saves you weeks of repetitive work so that you can focus more on your core mission. Let us handle your enrollment while you grow your practice!


Say goodbye to manual paperwork! Our automated system verifies credentials with accuracy and compliance—no hassle, no delays.

Track and monitor your credentialing process with instant notifications and zero guesswork. Stay informed every step of the way!

Expert support, customized for you! We make your operations smoother as our medical credentialing specialists assist you to ensure a smooth and hassle-free process.

Credentialing services in medical billing involve verifying a healthcare provider’s qualifications, licenses, and certifications to ensure they meet payer requirements. This service allows providers to enroll with insurance networks like Medicare, Medicaid, and private insurers. It includes CAQH registration, NPI enrollment, license verification, and payer contract negotiations. Get our efficient medical credentialing and ensure compliance, faster payments, and uninterrupted patient care.
Medical credentialing document requirements vary by insurance plan and payer. Generally, the following documents are required:
Credentialing allows providers to enroll with insurance networks. It enables them to bill and receive reimbursements for services. This process helps secure better-payer contracts and ensure higher and more timely reimbursements. Additionally, credentialing builds patient trust, attracts more patients, and increases overall revenue.
The provider enrollment process typically takes 80 to 120 days to complete. The credentialing time ultimately depends on the insurance company and how quickly they approve applications. However, we ensure an accurate and efficient submission to minimize delays on our end.
No, you must complete the credentialing process and receive approval from payers before you can bill for services. Treating patients without credentialing can result in denied claims, delayed payments, or compliance violations. It’s essential to complete this step to ensure smooth reimbursements and avoid disruptions in your practice.

30 mins meeting

Web conferencing details provided upon confirmation.
